A human osteoarthritis mimicking goat cartilage explant-based disease model for drug screening
Main Article Content
Abstract
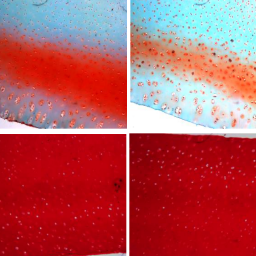
Although osteoarthritis (OA) is the most prevalent human joint disease with a large socioeconomic burden, it remains a neglected disease with no clinically approved disease modifying therapies. One of the key reasons for this is that the available disease models poorly recapitulate human OA-like traits, possibly because of the challenge of mimicking the disease in an ECM-rich cartilage tissue. In this study, we report the establishment and validation of a clinically relevant ex vivo OA model using IL1β-treated goat articular cartilage explants. Treatment with IL1β induced OA-like traits in goat cartilage explants and caused a shift in cartilage homeostasis towards enhanced catabolism, resulting in higher matrix degradation, overexpression of degradative and inflammatory mediators, and chondrocyte hypertrophy. We then validated the developed disease model for drug response using the drugs celecoxib, BMP7, and rapamycin, all of which demonstrated concentration-dependent disease amelioration in the model. Finally, we evaluated the translational relevance of the developed ex vivo OA model by comparing it with late-stage OA patient samples and observed a striking resemblance in terms of matrix degradation, expression of degradative enzymes, chondrocyte hypertrophy, and inflammation. Overall, the goat ex vivo OA model elicited a biological response to cytokine treatment that mirrors human OA-like traits and may reduce discordance between preclinical and clinical studies in OA drug development.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Articles are distributed under the terms of the Creative Commons Attribution 4.0 International license (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is appropriately cited (CC-BY). Copyright on any article in ALTEX is retained by the author(s).
Aigner, T., Fundel, K., Saas, J. et al. (2006). Large‐scale gene expression profiling reveals major pathogenetic pathways of cartilage degeneration in osteoarthritis. Arthritis Rheum 54, 3533-3544. doi:10.1002/art.22174
Barbosa, I., Garcia, S., Barbier-Chassefière, V. et al. (2003). Improved and simple micro assay for sulfated glycosaminoglycans quantification in biological extracts and its use in skin and muscle tissue studies. Glycobiology 13, 647-653. doi:10.1093/glycob/cwg082
Bhattacharjee, A., Kumar, K., Arora, A. et al. (2016). Fabrication and characterization of pluronic modified poly(hydroxybutyrate) fibers for potential wound dressing applications. Mat Sci Eng C Mater Biol Appl 63, 266-273. doi:10.1016/j.msec.2016.02.074
Bhattacharjee, A. and Katti, D. S. (2018). Pore alignment in gelatin scaffolds enhances chondrogenic differentiation of infrapatellar fat pad derived mesenchymal stromal cells. ACS Biomater Sci Eng 5, 114-125. doi:10.1021/acsbiomaterials.8b00246
Caramés, B., Hasegawa, A., Taniguchi, N. et al. (2012). Autophagy activation by rapamycin reduces severity of experimental osteoarthritis. Ann Rheum Dis 71, 575-581. doi:10.1136/annrheumdis-2011-200557
Chan, B., Fuller, E., Russell, A. et al. (2011). Increased chondrocyte sclerostin may protect against cartilage degradation in osteoarthritis. Osteoarthritis Cartilage 19, 874-885. doi:10.1016/j.joca.2011.04.014
Chang, S. H., Mori, D., Kobayashi, H. et al. (2019). Excessive mechanical loading promotes osteoarthritis through the gremlin-1-NF-κB pathway. Nat Commun 10, 1442. doi:10.1038/s41467-019-09491-5
Chubinskaya, S., Hurtig, M. and Rueger, D. C. (2007). OP-1/BMP-7 in cartilage repair. Int Orthop 31, 773-781. doi:10.1007/s00264-007-0423-9
Cope, P., Ourradi, K., Li, Y. et al. (2019). Models of osteoarthritis: The good, the bad and the promising. Osteoarthritis Cartilage 27, 230-239. doi:10.1016/j.joca.2018.09.016
Corciulo, C., Lendhey, M., Wilder, T. et al. (2017). Endogenous adenosine maintains cartilage homeostasis and exogenous adenosine inhibits osteoarthritis progression. Nat Commun 8, 15019. doi:10.1038/ncomms15019
Ding, L., Heying, E., Nicholson, N. et al. (2010). Mechanical impact induces cartilage degradation via mitogen activated protein kinases. Osteoarthritis Cartilage 18, 1509-1517. doi:10.1016/j.joca.2010.08.014
Feng, Z., Li, X., Lin, J. et al. (2017). Oleuropein inhibits the il-1β-induced expression of inflammatory mediators by suppressing the activation of NF-κB and mapks in human osteoarthritis chondrocytes. Food Funct 8, 3737-3744. doi:10.1039/c7fo00823f
Gabriel, N., Innes, J. F., Caterson, B. et al. (2010). Development of an in vitro model of feline cartilage degradation. J Feline Med Surg 12, 614-620. doi:10.1016/j.jfms.2010.03.007
Glyn-Jones, S., Palmer, A., Agricola, R. et al. (2015). Osteoarthritis. Lancet 386, 376-387. doi:10.1016/S0140-6736(19)30417-9
Han, B., Li, Q., Wang, C. et al. (2019). Decorin regulates the aggrecan network integrity and biomechanical functions of cartilage extracellular matrix. ACS Nano 13, 11320-11333. doi:10.1021/acsnano.9b04477
Hunter, D. J., Pike, M. C., Jonas, B. L. et al. (2010). Phase 1 safety and tolerability study of BMP-7 in symptomatic knee osteoarthritis. BMC Musculoskelet Disord 11, 232. doi:10.1186/1471-2474-11-232
Hunter, D. J., March, L. and Chew, M. (2020). Osteoarthritis in 2020 and beyond: A lancet commission. Lancet 396, 1711-1712. doi:10.1016/S0140-6736(20)32230-3
Johnson, C. I., Argyle, D. J. and Clements, D. N. (2016). In vitro models for the study of osteoarthritis. Vet J 209, 40-49. doi:10.1016/j.tvjl.2015.07.011
Kamisan, N., Naveen, S. V., Ahmad, R. E. et al. (2013). Chondrocyte density, proteoglycan content and gene expressions from native cartilage are species specific and not dependent on cartilage thickness: A comparative analysis between rat, rabbit and goat. BMC Vet Res 9, 62. doi:10.1186/1746-6148-9-62
Kapoor, M., Martel-Pelletier, J., Lajeunesse, D. et al. (2011). Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol 7, 33-42. doi:10.1038/nrrheum.2010.196
Karsdal, M., Michaelis, M., Ladel, C. et al. (2016). Disease-modifying treatments for osteoarthritis (DMOADs) of the knee and hip: Lessons learned from failures and opportunities for the future. Osteoarthritis Cartilage 24, 2013-2021. doi:10.1016/j.joca.2016.07.017
Le Graverand-Gastineau, M.-P. H. (2009). OA clinical trials: Current targets and trials for OA. Choosing molecular targets: What have we learned and where we are headed? Osteoarthritis Cartilage 17, 1393-1401. doi:10.1016/j.joca.2009.04.009
Li, Q., Han, B., Wang, C. et al. (2020). Mediation of cartilage matrix degeneration and fibrillation by decorin in post-traumatic osteoarthritis. Arthritis Rheumatol 72, 1266-1277. doi:10.1002/art.41254
Li, Y., Wang, Y., Chubinskaya, S. et al. (2015). Effects of insulin-like growth factor-1 and dexamethasone on cytokine-challenged cartilage: Relevance to post-traumatic osteoarthritis. Osteoarthritis Cartilage 23, 266-274. doi:10.1016/j.joca.2014.11.006
Little, C., Smith, M., Cake, M. et al. (2010). The OARSI histopathology initiative – Recommendations for histological assessments of osteoarthritis in sheep and goats. Osteoarthritis Cartilage 18, S80-S92. doi:10.1016/j.joca.2010.04.016
Little, C. B. and Hunter, D. J. (2013). Post-traumatic osteoarthritis: From mouse models to clinical trials. Nat Rev Rheumatol 9, 485-497. doi:10.1038/nrrheum.2013.72
Lohmander, L. S. and Roos, E. M. (2019). Disease modification in OA – Will we ever get there? Nat Rev Rheumatol 15, 133-135. doi:10.1038/s41584-019-0174-1
Lories, R. J. (2008). Joint homeostasis, restoration, and remodeling in osteoarthritis. Best Pract Res Clin Rheumatol 22, 209-220. doi:10.1016/j.berh.2007.12.001
Marotta, M. and Martino, G. (1985). Sensitive spectrophotometric method for the quantitative estimation of collagen. Anal Biochem 150, 86-90. doi:10.1016/0003-2697(85)90443-9
McCoy, A. M. (2015). Animal models of osteoarthritis: Comparisons and key considerations. Vet Pathol 52, 803-818. doi:10.1177/0300985815588611
McNulty, A. L., Rothfusz, N. E., Leddy, H. A. et al. (2013). Synovial fluid concentrations and relative potency of interleukin‐1 alpha and beta in cartilage and meniscus degradation. J Orthop Res 31, 1039-1045. doi:10.1002/jor.22334
Mengshol, J. A., Vincenti, M. P. and Brinckerhoff, C. E. (2001). IL-1 induces collagenase-3 (MMP-13) promoter activity in stably transfected chondrocytic cells: Requirement for Runx-2 and activation by p38 MAPK and JNK pathways. Nucleic Acids Res 29, 4361-4372. doi:10.1093/nar/29.21.4361
Mobasheri, A., Rayman, M. P., Gualillo, O. et al. (2017). The role of metabolism in the pathogenesis of osteoarthritis. Nat Rev Rheumatol 13, 302-311. doi:10.1038/nrrheum.2017.50
Murab, S., Chameettachal, S., Bhattacharjee, M. et al. (2013). Matrix-embedded cytokines to simulate osteoarthritis-like cartilage microenvironments. Tissue Eng Part A 19, 1733-1753. doi:10.1089/ten.tea.2012.0385
Netzel-Arnett, S., Mallya, S. K., Nagase, H. et al. (1991). Continuously recording fluorescent assays optimized for five human matrix metalloproteinases. Anal Biochem 195, 86-92. doi:10.1016/0003-2697(91)90299-9
Occhetta, P., Mainardi, A., Votta, E. et al. (2019). Hyperphysiological compression of articular cartilage induces an osteoarthritic phenotype in a cartilage-on-a-chip model. Nat Biomed Eng 3, 545-557. doi:10.1038/s41551-019-0406-3
Robinson, W. H., Lepus, C. M., Wang, Q. et al. (2016). Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis. Nat Rev Rheumatol 12, 580-592. doi:10.1038/nrrheum.2016.136
Roos, E. M. and Arden, N. K. (2016). Strategies for the prevention of knee osteoarthritis. Nat Rev Rheumatol 12, 92-101. doi:10.1038/nrrheum.2015.135
Saito, T. and Tanaka, S. (2017). Molecular mechanisms underlying osteoarthritis development: Notch and NF-κB. Arthritis Res Ther 19, 94. doi:10.1186/s13075-017-1296-y
Schneider, C. A., Rasband, W. S. and Eliceiri, K. W. (2012). NIH image to ImageJ: 25 years of image analysis. Nat Methods 9, 671-675. doi:10.1038/nmeth.2089
Shi, Y., Hu, X., Cheng, J. et al. (2019). A small molecule promotes cartilage extracellular matrix generation and inhibits osteoarthritis development. Nat Commun 10, 1914. doi:10.1038/s41467-019-09839-x
Siengdee, P., Radeerom, T., Kuanoon, S. et al. (2015). Effects of corticosteroids and their combinations with hyaluronanon on the biochemical properties of porcine cartilage explants. BMC Vet Res 11, 298. doi:10.1186/s12917-015-0611-6
Thudium, C. S., Engstrom, A., Groen, S. S. et al. (2019). An ex vivo tissue culture model of cartilage remodeling in bovine knee explants. J Vis Exp. doi:10.3791/59467
Ulivi, V., Giannoni, P., Gentili, C. et al. (2008). P38/ NF-κB‐dependent expression of COX‐2 during differentiation and inflammatory response of chondrocytes. J Cell Biochem 104, 1393-1406. doi:10.1002/jcb.21717
Van der Kraan, P. and Van den Berg, W. (2012). Chondrocyte hypertrophy and osteoarthritis: Role in initiation and progression of cartilage degeneration? Osteoarthritis Cartilage 20, 223-232. doi:10.1016/j.joca.2011.12.003
Wang, B., Chen, P., Jensen, A.-C. B. et al. (2009). Suppression of MMP activity in bovine cartilage explants cultures has little if any effect on the release of aggrecanase-derived aggrecan fragments. BMC Res Notes 2, 259. doi:10.1186/1756-0500-2-259
Wieland, H. A., Michaelis, M., Kirschbaum, B. J. et al. (2005). Osteoarthritis – An untreatable disease? Nat Rev Drug Discov 4, 331-344. doi:10.1038/nrd1693
Zhang, W., Ouyang, H., Dass, C. R. et al. (2016). Current research on pharmacologic and regenerative therapies for osteoarthritis. Bone Res 4, 15040. doi:10.1038/boneres.2015.40
Zweers, M. C., de Boer, T. N., van Roon, J. et al. (2011). Celecoxib: Considerations regarding its potential disease-modifying properties in osteoarthritis. Arthritis Res Ther 13, 239. doi:10.1186/ar3437